Guys Experience Pelvic Pain, Too. Here's How to Handle It.
Your Personal PT, Rachel Tavel, is a Doctor of Physical Therapy (DPT) and Certified Strength and Conditioning Specialist (CSCS) at Shift Wellness in NYC, so she knows how to get your body back on track when it’s out of line. In this weekly series, she gives you tips on how to feel better, get stronger, and train smarter.
Pain can come in many forms and affect any part of your body. That truly means any part of your body—even some areas you might not want to discuss. But know that if you are having pain in your most manly regions—particularly during your most intimate moments—you are not alone. Good news: there is a way to address your problem. The first step is understanding what’s wrong.
This pain in or around your junk is called pelvic pain. That refers to pain in the pelvis, lower abdomen, groin, genitals, perineum, rectum, buttocks, and even lower back area. Depending on what exactly is going on in your body, this type of pain can be felt during numerous daily activities, including during sex, urination, ejaculation, sitting, and exercise. Unfortunately, the global pandemic has created circumstances that may be contributing to an increase in symptoms, especially if you’re spending more time than ever sitting down indoors. I’ve called in some other experts to help you out.
Dr. Christian Reutter, DO, a physician with a specialty in pelvic rehabilitation medicine, and Dr. Erin Weber, PT, DPT, pelvic floor specialized doctor of physical therapy and founder of Flow Physiotherapy, have focused their careers on treating all different types of pelvic floor dysfunction and pain. They want you to know that you are not alone if you have pelvic pain—and there are things you can do right in your own home to address your symptoms.
What Is Pelvic Floor Dysfunction?
Pelvic floor dysfunction is often associated with women’s health and postpartum recovery, but it is also quite prevalent in men. Common pelvic pain conditions include: erectile dysfunction, prostatitis, urinary incontinence, levator ani syndrome, pudendal neuralgia, and chronic pelvic pain syndrome (among many others). While it sounds scary (and maybe not so sexy), don’t let it get you down. It doesn’t mean you’re damaged. You just need the right course of action.
Stocktrek ImagesGetty Images
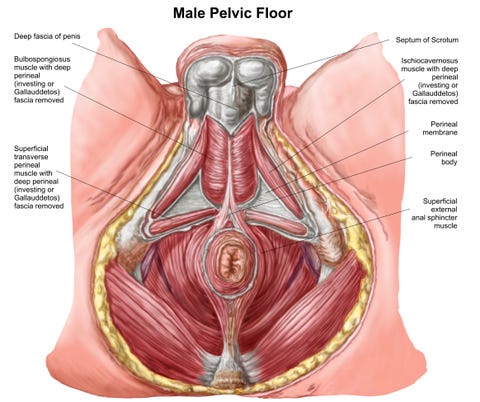
According to Dr. Reutter, the pelvic floor consists of a network of muscles that act as a “sling” to support the pelvic floor organs (the prostate, bladder, rectum and seminal vesicles), stabilize the connecting joints and assist in bladder, bowel and sexual function. Unlike the muscles you see when you hit the gym, these muscles are mostly internal and (hopefully) not visible to the general public. But they are critical to your everyday function and easily affected by stress, sleep, and other lifestyle factors.
With quarantine and a terrifying global pandemic in full-swing, many men are experiencing heightened symptoms. Dr. Weber believes this may be due to the current circumstances. “Quarantine and a global pandemic might just be the perfect storm for pelvic floor dysfunction.” Dr. Reutter adds that working from home, stress, uncertainty, sitting, lack of exercise, and lack of social connection contribute to any of these symptoms. According to Dr. Weber, the pelvic floor muscles often respond to our emotional state, acting as our human tail. During times of stress, fear and anxiety, we tend to ‘tuck our tails’ and contract our pelvic floors. Sitting on a couch or make-shift home office doesn’t help the situation.
How You Can Handle Pelvic Floor Dysfunction
To avoid this “perfect storm” of tension, Dr. Weber advises that you try to connect with your breath to help reduce any unwanted tension. “Taking deep belly breaths can reduce any pelvic floor gripping that might unconsciously happen in response to our current situation,” she advises.
Also, adjust how you’re sitting. Make sure you are sitting with your feet grounded, maintaining the neutral arch in your lower back. Try to “sit on your junk,” avoiding rolling back onto the SITS bones and slouching. Now take a big inhale and imagine that space relaxing. As you exhale, think of drawing that space together, lifting the scrotum. You should feel a contraction and subsequent relaxation of your pelvic floor muscles.

Roberto FoddaiGetty Images
In addition to breath work, Dr. Reutter suggests you take warm baths, increase aerobic activity (which increases endorphin levels, the body’s natural painkiller) and avoid prolonged sitting on hard surfaces to help relax the pelvic floor and mitigate symptoms. If you don’t respond to conservative treatment, injections could be administered to help break up the tension in the contracted pelvic floor muscles, reduce nerve inflammation, and improve blood flow to the affected region. But as tempting as injections might sound (ouch!), you’ll want to try conservative options such as physical therapy first.
Common Pelvic Floor Conditions

peakSTOCKGetty Images
Dr. Reutter and Dr. Weber go deep on a few common conditions below. If you are experiencing the symptoms described here, reach out to one of these experts to help determine the true cause of your symptoms and whether or not there is more you can do. If not addressed, your pelvic pain could have a large range of effects, from reducing your ability to produce power during your workout to impacting you emotionally and socially.
Prostatitis
The prostate is a small gland located directly below the bladder that enlarges over time. According to Dr. Reutter, prostatitis consists of swelling and inflammation of the prostate gland. This gland secretes a fluid that helps constitute semen or seminal fluid. Prostatitis can be bacterial or non-bacterial. Non-bacterial prostatitis is more common form and can be due to nerve irritation, chemical irritation, stress, and often a weak or spastic pelvic floor. Symptoms normally include painful urination, pain w ejaculation, and pain in the groin, genitals, and pelvic floor.
Levator Ani Syndrome
The levator ani is one of the muscles of your pelvic floor. It is primarily responsible for preventing urinary incontinence and supporting the pelvic organs. Dr. Reutter explains that this syndrome can be due to chronically contracted pelvic floor muscles.
Symptoms often present as pain in the rectum resulting in an “achy” feeling during and after intercourse, pain with bowel movements, constipation, and/or a feeling of rectal “fullness” or pain. Dr. Reutter notes: “Patients often describe a feeling of a ‘golf ball’ or similar in the rectum.” He adds that stress, anxiety, chronic constipation, a history of hemorrhoids, anal fissure, and prior colorectal surgery are all causes of levator ani syndrome.
Pudendal Neuralgia
Pudendal neuralgia is a condition that involves pain of the pudendal nerve, which runs from the anal region to the genitals. This condition is commonly associated with pinching or compression of the nerve. Symptoms include aching, burning, or stabbing pain in the penis or scrotum. This pain can increase with sitting and ejaculation.
Common causes are nerve entrapment, straining from bowel movements, trauma, and prolonged pressure on the pudendal nerve due to prolonged sitting on a hard surface, biking, and similar activities.
Chronic Pelvic Pain Syndrome (CPPS)
Anything “chronic” means you’ve been experiencing the pain for quite a while. Dr. Weber describes this syndrome as “pain over a longer duration of time, often causing discomfort with urination and ejaculation.” As a physical therapist, she usually finds patients have pain throughout the lower back/sacrum and lower abdomen/hip flexor/adductor muscle groups.
Men with CPPS undergo testing that rule out a bacterial infection, or are often given antibiotics as a trial for pain relief without success. “We find that the root of the pain is the overactive pelvic floor muscles.” To treat this type of overactivity, Dr. Weber creates a physical therapy plan consisting of reducing the muscle tension using manual therapy techniques applied to both the pelvic floor muscles and surrounding muscles/fascia throughout the pelvis (abdominals, hip flexors, adductors and deep hip rotators). Another important part of the intervention includes activity and exercise modification, along with postural education.
Men’s Health
Men’s Health Subscription
SHOP NOW
Source: Read Full Article
